Malignant growths (prostate cancer):
- May sometimes be a threat to life.
- Can spread to nearby organs and tissues (such as the bladder or rectum).
- Can spread (metastasize) to other parts of the body (like lymph nodes or bone).
- Often can be removed but sometimes grow back.
Cancerous cells of the prostate can multiply through dissociating from the prostate tumor. They are able to travel through blood vessels, or lymph nodes to connect with other organs of the body. After spreading, cancer cells may attach to other tissues and grow to form new tumors, causing damage where they land.
When prostate cancer spreads from its original place to another part of the body, the new tumor has the same kind of abnormal cells and the same name as the primary tumor. For example, if prostate cancer is spread to the bones, then the cancer bone tissue contains in fact prostate cancerous cells. The cause is metastatic prostate cancer, not bone cancer. It's treated as bone cancer of the prostate.
Symptoms
In the early stages of its development prostate cancer is often characterized by no signs. If there are symptoms they may be similar to the symptoms of an enlarged prostate, or BPH. Prostate cancer may also trigger symptoms that aren't related to BPH.
Symptoms of prostate cancer can be:
- Dull pain in the lower pelvic area
- Frequent urinating
- Trouble urinating, pain, burning, or weak urine flow
- Blood in the urine (Hematuria)
- Painful ejaculation
- Pain in the lower back, hips or upper thighs
- Loss of appetite
- Loss of weight
- Bone pain
Prostate Cancer Risk Factors
Risk factors are any thing which increases the risk of developing a disease, like cancer. Different types of cancer have different risk factors. Certain risk factors, such as cigarettes, are able to be altered. Other things, such as a person's background or age cannot be altered. Others, like a person’s age or family history, can’t be changed.
However, the presence of a risk factor or even a few isn't a guarantee that you'll contract the disease. A lot of people who have some risk factors will never develop cancer. However, those who do get cancer might have had no or few known risk factors. Researchers have identified a variety of variables that could impact the risk for men to develop prostate cancer.
-
Age
Prostate cancer is not common for men who are younger than 40 years old however the likelihood of developing prostate cancer increases dramatically after the age of 50. Six out of 10 prostate cancer cases occur in older men.
-
Race/ethnicity
Prostate cancer is more common in African American males and Caribbean men with African descent than people of other races. If it develops in these males, they tend to be younger. Prostate cancer is less common when you are Asian American and Hispanic/Latino men as compared to non-Hispanic whites. The reason for these racial and ethnic distinctions aren't entirely evident.
-
Geography
Prostate cancer is the most prevalent throughout North America, northwestern Europe, Australia, and on Caribbean islands. It is more rare it is less common in Asia, Africa, Central America as well as South America.
The reason for this is unclear. A more thorough screening for prostate cancer in some nations could be responsible for at least a part of this variation, but other factors, such as lifestyle changes (diet and lifestyle, etc.) are also a factor. is likely to be significant also. For instance, Asian Americans have a lower risk of contracting prostate cancer than non-Asian Americans However, their risk is greater than men with similar ethnic backgrounds who live in Asia.
-
Family history
Prostate cancer appears to be prevalent in certain families, suggesting that in certain cases, there could be an inheritance or genetic component. Yet, the majority of prostate cancers are found in males with no family record of it.
A brother or father suffering from prostate cancer can more than double the risk for a man to develop the cancer. (The risk is greater for those who have one brother suffering from the disease than those with one of their parents with it.) The risk is more pronounced for males. with multiple relatives affected who have a number of relatives affected, especially if the relatives were children when the cancer was discovered.
-
Gene changes
Several inherited gene changes (mutations) seem to raise prostate cancer risk, but they probably account for only a small percentage of cases overall. For example: Genetic mutations within genes like the BRCA1 as well as BRCA2 genes that are associated with an increase in risk for developing breast and ovarian cancers within certain families, also can increase the risk of prostate cancer. Cancer risk for men (especially the mutations that affect BRCA2).
Men who suffer from Lynch syndrome (also called hereditary non-polyposis colorectal carcinoma, or HNPCC) is a condition that is caused by genetic changes, are at a higher risk of developing several cancers, such as prostate cancer.
Other genetic changes that are inherited can increase a man's chances of developing prostate cancer. For more on some of these gene changes, Factors with less clear effects on prostate cancer risk
-
Diet
The exact role of diet in prostate cancer is not clear, but several factors have been studied.
Men who eat a lot of dairy products appear to have a slightly higher chance of getting prostate cancer.
Some studies have suggested that those who consume a large amount of calcium (through supplements or food) could be at a greater likelihood in being diagnosed with prostate cancer. But the majority of studies have not discovered a connection between the amount of calcium present in our typical diets and it's vital to keep in mind that calcium is widely known to There are many other health benefits.
-
Obesity
Being overweight (very overweight) doesn't seem to increase the likelihood of developing prostate cancer.
Some A few studies have revealed that overweight men are at a lower risk of developing a low-grade (slower developing) type of the disease. However, they do have an increased risk of becoming more aggressive (faster Growing) prostatic cancer. The reasons behind the growth of prostate cancer are not known.
Some studies have also shown that overweight men are more at risk of developing an advanced form of prostate cancer as well as of dying from prostate cancer however, not all studies have shown this. This is what I found.
-
Smoking
The majority of studies haven't found a connection between smoking cigarettes and developing prostate cancer. Some research has linked smoking to a possible small increased risk of dying from prostate cancer, but this finding needs to be confirmed by other studies.
-
Chemical exposures
There is evidence to suggest that firefighters may be exposed to chemicals which could increase their risk of developing prostate cancer.
A few studies have suggested a possible link between exposure to Agent Orange, a chemical used widely during the Vietnam War, and the risk of prostate cancer, although not all studies have found such a link. The National Academy of Medicine considers there to be “limited/suggestive evidence” of a link between Agent Orange exposure and prostate cancer.
-
Inflammation of the prostate
Some studies have suggested that prostatitis (inflammation of the prostate gland) may be linked to an increased risk of prostate cancer, but other studies have not found such a link. Inflammation is often seen in samples of prostate tissue that also contain cancer. The link between the two is not yet clear, and this is an active area of research.
-
Sexually transmitted infections
Researchers have investigated whether sexually transmitted infections (like the chlamydia and gonorrhea) may increase the chance of developing prostate cancer because they may cause an inflammation in the prostate. As of now, research has not been conclusive with the findings, and no definitive conclusions have been drawn.
-
Vasectomy
Certain studies have suggested that those who've been through vasectomy (minor procedure to make men infertile) have a slight increase in risk of prostate cancer however other studies haven't confirmed this.
Tests to Diagnose and Stage Prostate Cancer
Medical history and physical exam
If your doctor suspects you might have prostate cancer, you will be asked about symptoms you are having, such as any urinary or sexual problems, and how long you have had them. You could be asked about any possible risk factors, like the family history of your parents.
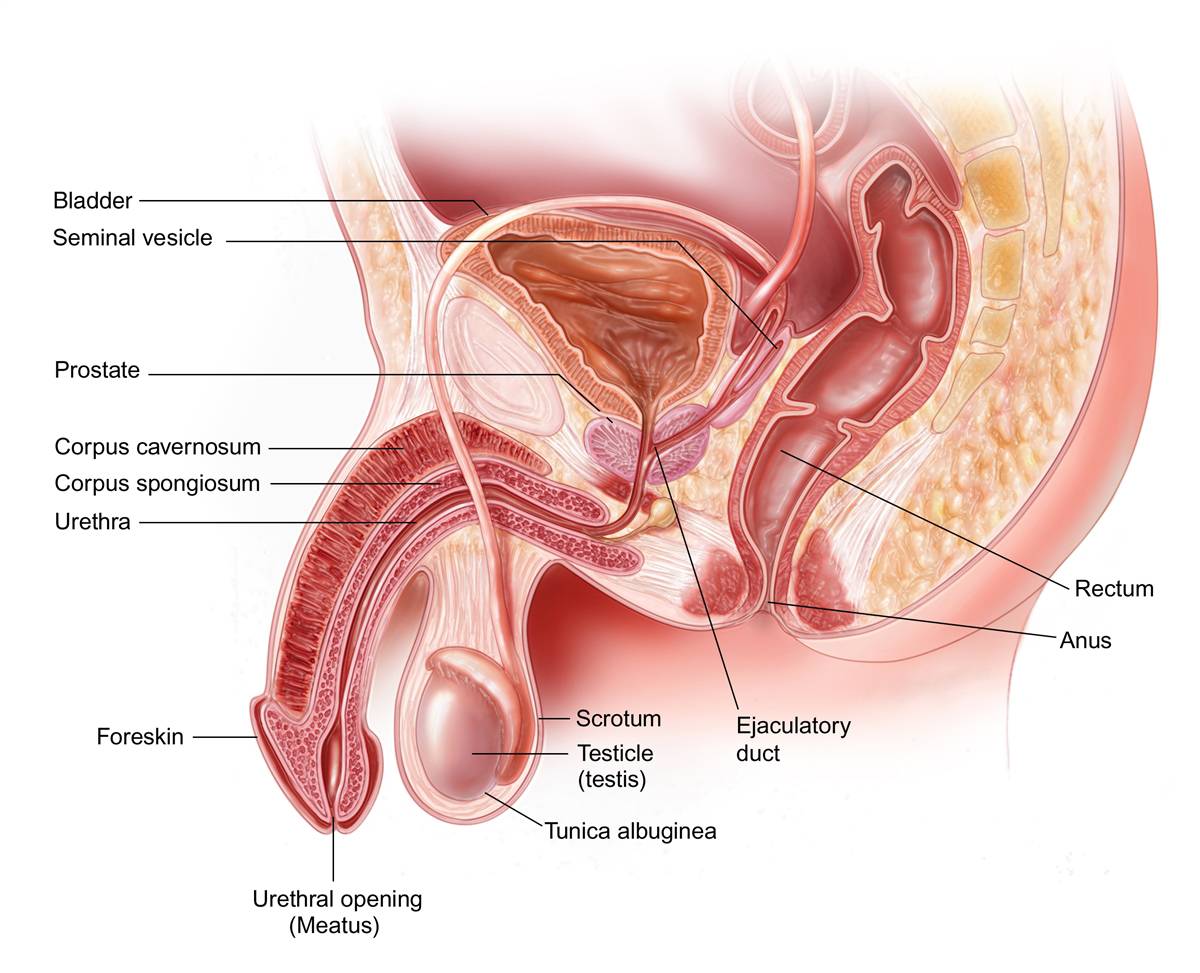
Your doctor will also examine you. It could also be a digital rectal examination (DRE) where doctors insert a gloved lubricated hand into your rectum, allowing them to detect any hard or bumpy areas on the prostate which may is cancerous. If you do have cancer, the DRE can sometimes help tell if it’s only on one side of the prostate, if it’s on both sides, or if It is believed that the cancer has expanded beyond the prostate to adjacent tissues. Your doctor might also look at other parts in your body.
After your exam the doctor may decide to order tests.
PSA blood test
Prostate-specific Antigen (PSA) is a protein produced by prostate cells. gland (both normal cells as well cancerous cells). PSA is mostly found in semen, but a smaller amount can also be found in blood.
It is a PSA tests for blood are employed predominantly to test for prostate cancer in men with no any symptoms. It's also among the first tests performed in patients who show signs that could be due to prostate cancer. A lot of doctors employ the PSA cutoff level that is 4 ng/mL or more in determining if a person may require additional testing. Other doctors might suggest beginning at the level of Lower levels, for instance 2.5 or 3.
Most prostate cancer patients have PSA levels below 4 ng/mL blood. However, a blood test that is lower than 4 doesn't mean that a person doesn't have cancer.Most prostate cancer patients have PSA levels below 4 ng/mL blood. However, a blood test that is lower than 4 doesn't mean that a person doesn't have cancer.
Men who have an PSA range that is between 4-10 (often known as"borderline range "borderline area") have around one in four possibility of developing prostate cancer. If the PSA is higher than 10, the probability of developing prostate cancer is greater than 50 percent.
If your PSA level is high, you might need further tests to look for prostate cancer.
The PSA test can also be useful if you have already been diagnosed with prostate cancer.
For men who have just been confirmed with cancer of the prostate The PSA levels can be analyzed in conjunction with the results of a physical exam and the tumor grade (determined through a biopsy, which is described in detail on) to assist Determine if further test (such such as CT scans, Bone scans) are required.
The PSA level is used to help determine the stage of your cancer. This can affect your treatment options, since some treatments (such as surgery and radiation) are not likely to be helpful if the cancer has spread to other parts of the body.
PSA tests are usually an essential element in understanding how well the treatment is working and also to look out for a potential return of cancer following treatment.
Prostate biopsy
When the findings of the PSA tests, DRE as well as other diagnostic tests indicate that you may have prostate cancer, then you are most likely to require an examination of your prostate. A biopsy is a procedure in which small samples of the prostate are removed and then looked at with a microscope. A needle biopsy of the core is the primary method for diagnosing prostate cancer. The procedure is typically performed by an urologist.
During the biopsy, the doctor usually looks at the prostate with an imaging test such as transrectal ultrasound (TRUS) or MRI, or a ‘fusion’ of the two (all discussed below). The doctor inserts a small, hollow needle through the prostate. It can be done by a biopsy of the rectum (a transrectal biopsy) or by removing it through the skin between the scrotum as well as the anus (a transperineal biopsies). When the needle is pulled out it removes a small cylinder (core) of prostate tissue. The doctor will typically collect about 12 core samples from various areas in the prostate.
The majority of doctors who conduct the biopsy will numb prostate first, by injecting a local anesthetic beside the prostate. You might want to ask your doctor if there are plans to do this.
The procedure itself can take about 10 minutes, and is typically performed in the office of a doctor. The chances are that you'll be offered antibiotics to consume prior to the biopsy, and perhaps for a few days following the procedure to lower the risk of getting a infection. After a few days of your procedure could notice some soreness in the area, and may detect some blood of your urine. You might also experience slight bleeding from your rectum, particularly when you suffer from hemorrhoids. A lot of men find semen that is bloody or have semen with rust-colored pigments that lasts for a few weeks following the biopsy, based on how often you exhale.
Getting the results of the biopsy
Your biopsy samples will be sent to a lab, where they will be looked at with a microscope to see if they contain cancer cells. Getting the results (in the form of a pathology report) usually takes at least 1 to 3 days, but it can sometimes take longer. The results might be reported as:
Positive for cancer: The cells of cancer were detected on the tissue samples for biopsy.
Negative for cancer: No cancerous cells were found within the samples of biopsy.
Suspicious:A suspicious sign was observed, however it could not be cancer.
(Different kinds of results that are suspicious are discussed in the following section.)
If the biopsy is negative
If the results of a prostate biopsy are not positive (that is, they don't reveal cancer) The probability that you've got prostate cancer isn't that excessive based upon your PSA level as well as the other ones, so you may be able to skip any tests, except for repeated PSA tests (and maybe DREs) in the future. However, even if a lot of biopsies are taken, they are not guaranteed to detect cancer if no biopsy needles are able to pass through it. This is referred to as a false negative result. If your doctor is still believes that you may have prostate cancer (because your PSA level is extremely high, for instance) Your doctor may suggest:
Other lab tests (of urine, blood or prostate biopsy sample) to give you an idea of the possibility that you be suffering from prostate cancer. Some examples of such tests are tests like the Prostate Health Index (PHI) Test, 4Kscore PCA3 tests, and ConfirmMDx. The test is discussed in the article What's New within Prostate Cancer Research?
A repeat prostate biopsy. This may include taking additional prostate samples from areas of the prostate that weren't previously biopsied or using imaging tests like MRI (described further below) to examine the prostate more closely. For areas with abnormalities to focus on
Prostate cancer grade (Gleason score or Grade Group)
In the event that prostate cancer discovered in an x-ray the cancer will be classified. The degree of cancer is determined by how unusual the cancer appears under a microscope. Cancers with higher grades appear more bizarre and are more likely to develop and spread rapidly. There are two primary ways to describe the degree of prostate cancer.
Gleason score
The Gleason system that has been used for a long time is a system that assigns grades according to how much the cancer appears similar to regular prostate tissues. If the cancer appears much like normal prostate tissue the grade 1 is given.
If the cancer appears unusual, it's assigned the grade 5. Grades 2 through 4 contain characteristics that fall between these extremes. The majority of cases of cancer are in grade 3 or greater Grades 1 and 2 aren't frequently utilized.
As prostate cancers usually contain areas of different grade A grade is given to the two areas which make up the bulk parts of prostate cancer. These two grades are combined to produce what is known as the Gleason score (also known as"the Gleason Sum). The first number that is assigned is the grade most prevalent in the tumor. For example, if a Gleason score was written 3+4=7 it indicates that the majority of the tumors are grade 3 and less than that is grade 4, and the tumors are then added to create an Gleason score of 7.
Though most of the time, Gleason score is determined by two areas that comprise the majority part of the tumor, there may be cases where a biopsy sample contains a significant amount of high-grade cancer, or there are three grades, including high-grade cancer. In these situations the method by which how the Gleason score is calculated can be altered so that it reflects an extremely aggressive (fast-growing) characteristics of cancer.
In theory, the Gleason score can be between 2 and 10, but scores below 6 are rarely used.
Based on the Gleason score, prostate cancers are often divided into 3 groups:
Cancers with a Gleason score of 6 or less may be called well-differentiated or low-grade. Cancers with a Gleason score of 7 may be called moderately-differentiated or intermediate-grade. Cancers with Gleason scores of 8 to 10 may be called poorly-differentiated or high-grade.
Grade Groups
In recent years, doctors have come to realize that the Gleason score might not always be the best way to describe the grade of the cancer, for a couple of reasons:
Prostate cancer outcomes can be divided into more than just the 3 groups mentioned above. For example, men with a Gleason score 3+4=7 cancer tend to do better than those with a 4+3=7 cancer. And men with a Gleason score 8 cancer tend to do better than those with a Gleason score of 9 or 10.
The scale of the Gleason score can be misleading for patients. For example, a man with a Gleason score 6 cancer might assume that his cancer is in the middle of the range of grades (which in theory go from 2 to 10), even though grade 6 cancers are actually the lowest grade seen in practice. This assumption might lead a man to think his cancer is more likely to grow and spread quickly than it really is, which might affect his decisions about treatment.
Because of this, doctors have developed Grade Groups, ranging from 1 (most likely to grow and spread slowly) to 5 (most likely to grow and spread quickly):
Grade Group 1 = Gleason 6 (or less)
Grade Group 2 = Gleason 3+4=7
Grade Group 3 = Gleason 4+3=7
Grade Group 4 = Gleason 8
Grade Group 5 = Gleason 9-10
The Grade Groups will likely replace the Gleason score over time, but currently you might see either one (or both) on a biopsy pathology report.
Other information in a pathology report
Along with the grade of the cancer (if it is present), the pathology report often contains other information about the cancer, such as:
The number of biopsy core samples that contain cancer (for example, “7 out of 12”)
The percentage of cancer in each of the cores
Whether the cancer is on one side (left or right) of the prostate or on both sides (bilateral)
Suspicious results
Sometimes when the prostate cells are seen, they don’t look like cancer, but they’re not quite normal, either.
Prostatic intraepithelial neoplasia (PIN): In PIN, there are changes in how the prostate cells look, but the abnormal cells don’t look like they’ve grown into other parts of the prostate (like cancer cells would). PIN is often divided into 2 groups:
Low-grade PIN: The patterns of prostate cells appear almost normal.
High-grade PIN: The patterns of cells look more abnormal.
Many men begin to develop low-grade PIN at an early age, but low-grade PIN is not thought to be related to prostate cancer risk. If low-grade PIN is reported on a prostate biopsy, the follow-up for patients is usually the same as if nothing abnormal was seen.
If a high-grade PIN has been identified during an ultrasound, there is an increased likelihood that you will develop prostate cancer in the future. This is the reason why doctors monitor men with PIN that is high-grade and are able to recommend a prostate biopsy (or laboratory tests) to aid in determining the likelihood of developing cancer). as as the Prostate Health Index (PHI) as well as the 4Kscore test, such as the PCA3 Test (such like Progensa) as well as ConfirmMDx). This is particularly true when high-grade PIN is detected in multiple areas in the prostate (multifocal high-grade PIN) or if the initial biopsy was not taken from all Parts of the prostate.
Atypical small acinar growth (ASAP) It could be referred to as glandular atypia or an atypical proliferative. It could also be described to be "suspicious as a cancer." These words mean the cells appear to could be cancerous when examined under a microscope. But there aren't enough of them to say for certain. If any or more of the terms above is mentioned then there's a good chance that you have prostate cancer and that's why many doctors suggest conducting a biopsy again within A couple of months. Proliferative inflamma-tive atrophy (PIA) In PIA prostate cells, they appear smaller than normal and there are indications of inflammation within the area. PIA isn't cancer however, research suggests that PIA can result in high-grade PIN or prostate cancer in the first instance.
For more details on the way the results of prostate biopsy are reported, please visit this section of our website. Prostate Pathology section on our website.
Genetic testing is available for certain men suffering from prostate cancer.
Certain doctors are now suggesting that men suffering from prostate cancer should be screened to determine if they have genes that have been inherited. This includes people with there is a family cancer-related syndrome (such as the BRCA gene variant as well as Lynch syndrome) is thought to be present or diagnosed, as well as those who are diagnosed with prostate cancer. certain risky features or is spreading to other parts in the human body. Discuss with your physician the potential pros and disadvantages, and possible limitations of this type of test.
Imaging tests for prostate cancer
Transrectal ultrasound (TRUS)
Magnetic resonance imaging (MRI)
Positron emission tomography (PET) scan
Computed tomography (CT) scan
Lymph node biopsy
Lymph node biopsy as a separate procedure